From WVU Today:
MORGANTOWN, W.Va. — It may seem that the COVID-19 vaccine came from out of nowhere, but it actually underwent the same rigorous testing that all vaccines do. It’s safe. It’s effective. And it represents a huge step toward making life feel normal again, according to one West Virginia University vaccine expert.
In fact, the development of COVID-19 vaccines did not begin at the onset of the pandemic itself. Scientists have researched vaccines over the years for related coronaviruses, such as SARS and MERS, and the timing and effort have now fallen into place.
“With the technology that we have right now, we were able to create this vaccine faster, but this vaccine went through the same testing phases as any other vaccine that was developed before,” said Ivan Martinez, an associate professor in the WVU School of Medicine and Cancer Institute.
Before the Food and Drug Administration approves a vaccine for use, it has already undergone rigorous testing at the molecular scale, in animals and in people who volunteer to participate in trials.
The COVID-19 vaccine is no different.
Making wheels, not building cars
The COVID-19 vaccine could run the gauntlet of tests so quickly because scientists conducted all three phases of clinical trials simultaneously rather than sequentially.
Another reason the vaccine could be ready so fast was the innovative way scientists produced it in the lab, Martinez said.
The traditional process is tedious. First, scientists have to identify and isolate the virus. Then they have to figure out what type of cells they can grow the virus in. After that, they nurture the virus in a laboratory setting as it multiplies over countless generations. If all goes according to plan, the virus can infect an animal model (like mice, guinea pigs or monkeys) so that the scientists can manipulate them and use these viruses for a vaccine.
“Imagine that a virus is like a car,” Martinez said. “When we were developing vaccines the traditional way, it was as if we created these cars artificially in the lab without putting in the engine. Then we put this car inside of our bodies. Our immune system would detect the car, chop it up into little pieces and create antibodies for different parts of the car: an antibody against the windshield, an antibody against the bumper, an antibody against the wheels.”
This time, scientists didn’t rely on whole virus cells to make the vaccine. Instead they used a snippet of the virus’ messenger RNA, the instructions cells follow to build proteins. Messenger RNA is less like a car and more like the blueprint for its tires.
“So you put this blueprint inside our cells, and our cells start making the tires,” Martinez said. “Our immune system detects those tires—because they don’t look like they belong to us—and creates antibodies against them. They’re very safe because there’s no way you can get infected from just the tires. There’s no engine; there’s no bumper; there’s no windshield. There’s no car.”
The messenger RNA can’t integrate with our DNA, so there’s no need to worry that it will alter our genetic makeup. And it disappears after only a few days, which means it won’t linger in our cells after fulfilling its purpose.
‘Don’t feel like you’re a guinea pig’
So far, side effects of the vaccine have been rare.
Two people in the United Kingdom and one in Alaska experienced allergic reactions after receiving the Pfizer/BioNTech vaccine. But Martinez emphasizes that those three individuals make up a tiny portion of the total number of vaccine recipients.
According to the FDA, only 1% of study participants who received the Moderna vaccine experienced serious adverse events, a frequency that the FDA deems “low.” That’s identical to the rate of serious adverse events in people who received a placebo.
And in a trial of the vaccine that Pfizer/BioNTech developed, just 0.6% of people in the vaccine group—and 0.5% of people in the placebo group—had at least one serious adverse event.
“Please don’t feel like you’re a guinea pig,” Martinez said. “It’s clearly safe.”
Goodbye, 2020! Hello, 2021!
How long will our immune system remember the vaccine and protect us against the virus?
“Nobody really knows,” Martinez said. “With other types of coronaviruses—like the ones that cause the common cold—we create antibodies against them for only a few years. So, we’ll probably get a coronavirus vaccine every year, just like the influenza vaccine.”
The good news is, scientists will be able to tweak the vaccine formulation in response to the virus’s mutations over time. In doing so, they can preserve the vaccine’s effectiveness in the years to come.
As effective as the vaccine is, people will still need to practice social distancing and wear masks after they receive it—at least, for now.
Scientists are confident that the vaccine keeps people from coming down with COVID-19, but they don’t yet know if it prevents people from passing the virus onto others. There simply isn’t enough data.
According to estimates, we won’t achieve herd immunity until 70% to 80% of the population has been vaccinated.
“We have to be aware that, even when we get to that point, we still have to keep our distance, and we still have to wear masks, probably until the fall of this coming year,” Martinez said. “But during this time, hopefully most of the population will get vaccinated. And then, hopefully next Christmas will be back to normal.”
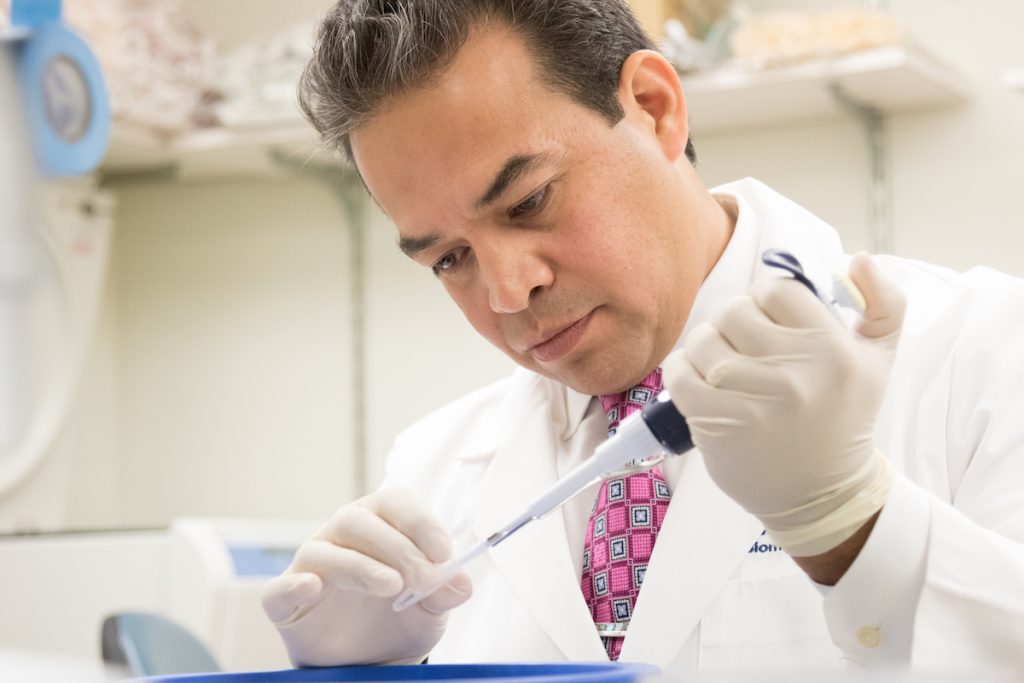
Dr. Ivan Martinez, a virologist and associate professor in the WVU School of Medicine, talks through a few of the myths about the COVID-19 vaccine.






